Valvular disease in dogs, particularly in giant breeds, is a significant health concern that requires attention and understanding. While degenerative valve disease (DVD) is more commonly associated with smaller breeds, large and giant breed dogs are not immune to this condition. DVD is the most prevalent heart disease in canines and a leading cause of congestive heart failure (CHF).
In giant breed dogs, the pathophysiology of DVD can be quite complex. The disease often progresses over many years, and its morbidity is directly related to the degree of valvular insufficiency and subsequent volume overload to the heart. The mitral valve is most commonly affected, though the tricuspid valve may also be involved. The structural changes in the valve leaflets, the integrity of the chordae tendineae, myocardial contractility, and chamber dilation all contribute to the progression of valvular regurgitation and eventually lead to heart failure.
The compensatory mechanisms that come into play as the disease progresses are fascinating yet concerning. As valve regurgitation worsens, the forward cardiac output diminishes, stimulating various compensatory mechanisms to ensure the circulatory needs of the body are met. This primarily involves an increase in preload (Frank-Starling relationship). However, these compensatory changes can only maintain the dog’s health for a certain period before the risk of developing edema or CHF increases.
For giant breed dog owners, it’s crucial to be aware of the symptoms and seek veterinary care if they suspect their pet may be suffering from valvular disease. Early detection and treatment can significantly improve the quality of life for these dogs. Symptoms can include a persistent cough, lethargy, difficulty breathing, and reduced tolerance for exercise. A veterinary cardiologist can provide a thorough examination, including echocardiography, to assess the condition of the heart valves and chambers.
Treatment options for valvular disease in dogs may include medications to manage heart failure symptoms and improve heart function. In some cases, surgical interventions such as valve repair or replacement may be considered, although these are less common in veterinary medicine compared to human medicine.
Research continues to advance our understanding of DVD in dogs of all sizes, and ongoing studies aim to improve the management and treatment of this condition. For instance, a study published in 2024 highlighted the survival rates and management strategies for myxomatous mitral valve disease (MMVD) in large breed dogs, providing valuable insights for veterinarians and pet owners alike.
In conclusion, while valvular disease is a serious health issue in giant breed dogs, advancements in veterinary cardiology offer hope for better management and treatment options. Owners of giant breed dogs should work closely with their veterinarians to monitor their pets’ heart health and take proactive steps to address any signs of heart disease early on. With proper care and attention, dogs with valvular disease can continue to lead fulfilling lives. For more detailed information on this topic, please refer to the resources provided.
Definition
Clinical Definition:
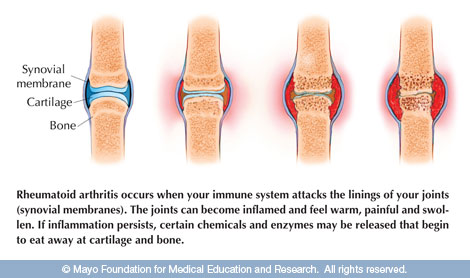
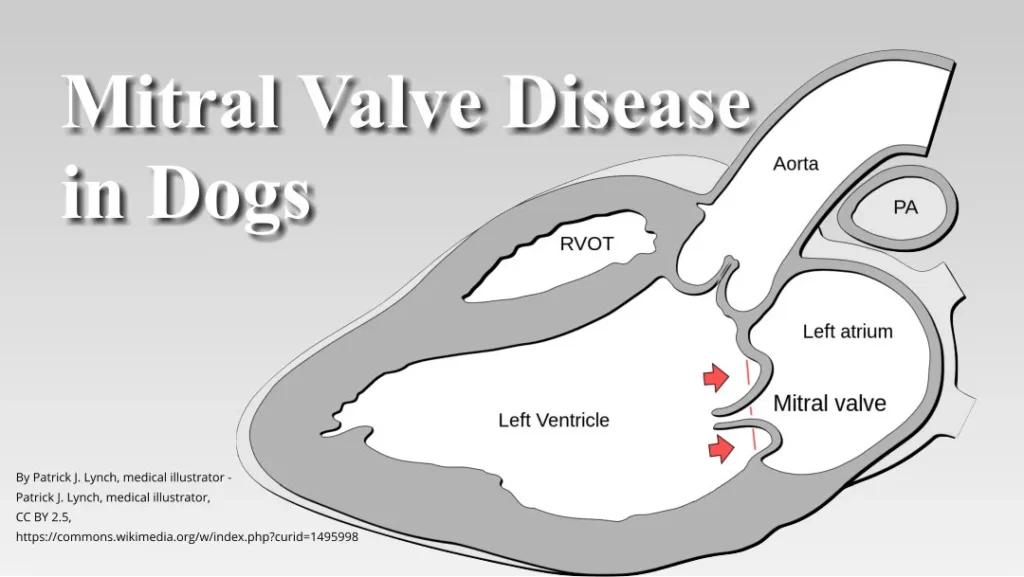
Mitral Valve Disease (MVD) is a progressive cardiac condition characterized by degeneration or malfunction of the mitral valve. This leads to incomplete closure of the valve, allowing blood to flow backward into the left atrium, a condition known as mitral regurgitation. Over time, this can cause heart enlargement, reduced cardiac efficiency, and eventual heart failure.
Layman’s Definition:
The mitral valve is like a door that keeps blood flowing the right way in the heart. Mitral Valve Disease happens when that door gets weak or leaky, letting blood slip backward instead of moving forward like it should. This makes the heart work extra hard, like trying to pump water with a broken hose.
How Mitral Valve Disease Affects the Heart
In a healthy heart, the mitral valve ensures that blood flows smoothly from the left atrium into the left ventricle, which pumps oxygen-rich blood out to the body. When the mitral valve is damaged or weakened, it doesn’t close tightly, allowing blood to leak backward into the atrium (mitral regurgitation). This leakage increases the heart’s workload as it must pump harder to maintain adequate blood flow to the body. Over time, this extra strain can lead to:
- Heart enlargement (left atrial and ventricular dilation): The heart stretches to handle the increased blood volume.
- Congestive heart failure: The heart’s ability to pump blood effectively diminishes, leading to fluid buildup in the lungs and other parts of the body.
- Reduced oxygen delivery: The backward flow of blood disrupts efficient circulation, causing fatigue and shortness of breath.
Symptoms
Symptoms of Mitral Valve Disease in Dogs
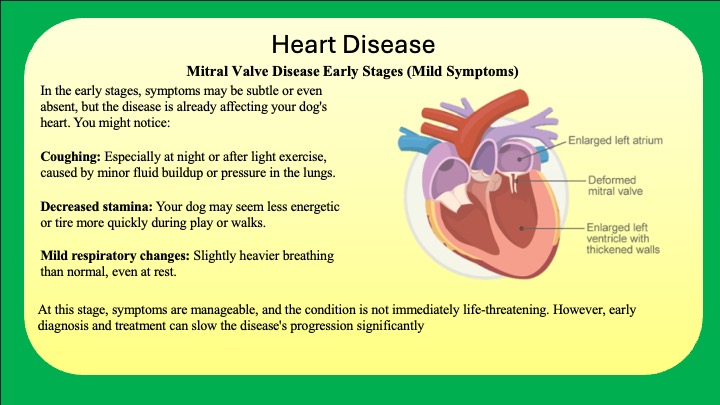
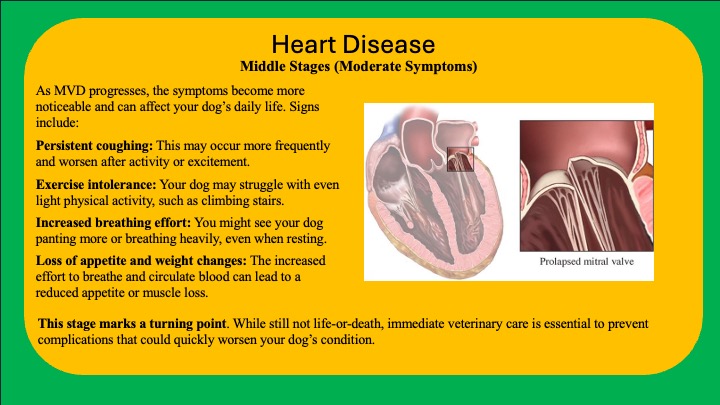
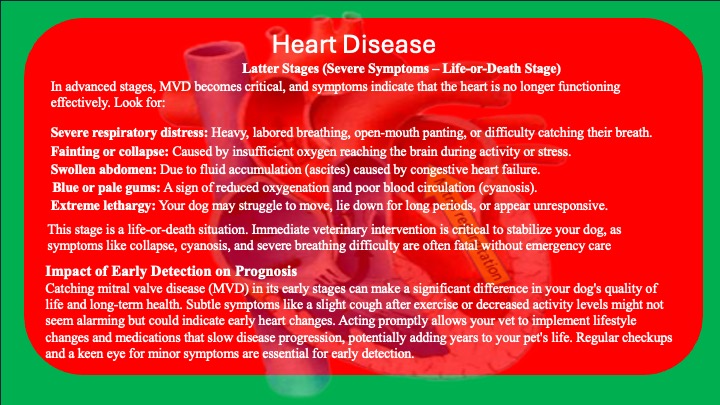
Mitral Valve Disease (MVD) progresses gradually, and its symptoms change as the condition advances. As a dog owner, recognizing these stages can help you act promptly to ensure your pet’s health and well-being. Here’s what to expect in each phase:
Health Tracking Apps
When to Call the Vet
At the first signs of symptoms (even in the early stage), you should consult your veterinarian. Early diagnosis and treatment can dramatically improve your dog’s quality of life and slow the disease’s progression. However, if your dog reaches the latter stage and exhibits severe symptoms, it is an emergency, and immediate action is required to save their life.
Interactive Elements or Tools
A Symptom Tracker (links in the Symptoms section) can guide owners in recording coughing frequency, energy levels, and appetite changes.
Prevention
Preventive Measures for Mitral Valve Disease in Dogs
Mitral Valve Disease (MVD) is often linked to genetics and age, meaning prevention isn’t always possible. However, there are proactive steps owners can take to support heart health and potentially reduce the risk of severe complications.
1. Regular Veterinary Check-Ups
Routine vet visits can catch early signs of MVD, especially in breeds predisposed to the condition, such as Cavalier King Charles Spaniels, Dachshunds, and Miniature Poodles. Annual heart exams, including listening for murmurs, are critical for early detection.
2. Maintain a Healthy Weight
Obesity puts additional strain on your dog’s heart. Feed a balanced diet tailored to your dog’s breed, size, and activity level. Avoid excessive treats and monitor their weight closely.
3. Provide Regular Exercise
Moderate, consistent exercise keeps your dog’s heart strong. Avoid overexertion, especially in breeds at higher risk of MVD.
4. Monitor for Symptoms
Coughing, reduced energy, or labored breathing should never be ignored. Early intervention slows the disease’s progression.
5. Use Preventive Medications if Recommended
For dogs at high risk, some vets may prescribe medications to support heart function and reduce strain on the valves.
While you can’t prevent MVD entirely, focusing on heart health and working with your vet can improve your dog’s quality of life and help delay disease onset.
Just Like with humans
Preventing Mitral Valve Disease in dogs is quite similar to maintaining heart health in humans. Key actions like weight control, regular exercise, a balanced diet, and routine health check-ups are just as important for dogs as they are for people.
These measures don’t necessarily prevent the disease entirely, especially if it’s due to genetic factors or age, but they help reduce strain on the heart and delay the progression of symptoms. Think of it as giving your dog the best possible foundation for a healthy heart, even if predisposition to MVD is unavoidable.
Interactive Elements or Tools
A Weight and Diet Calculator (linked in the Prevention section) can assist in managing a healthy weight for your dog.
Products to Help
While no products can directly prevent Mitral Valve Disease (MVD), several can support heart health and overall well-being, potentially delaying the onset or progression of heart-related issues. Here are a few categories of products that may help:
1. Heart-Healthy Supplements
- Omega-3 Fatty Acids: Found in fish oil supplements, they support cardiovascular health by reducing inflammation and improving blood flow.
- Coenzyme Q10 (CoQ10): An antioxidant that helps with cellular energy production and may support heart muscle function.
- Taurine and L-Carnitine: Amino acids that promote heart health, particularly in breeds prone to cardiac issues.
2. Weight Management Tools
- Low-Calorie Treats: Help control calorie intake while keeping your dog happy.
- Portion-Control Feeders: Automatically measure food portions to prevent overfeeding.
- High-Quality Dog Food: Choose a diet formulated for heart health, often labeled as “cardiac care” or “low sodium.”
3. Exercise and Monitoring Aids
- Activity Monitors: Track your dog’s activity levels to ensure they’re getting the right amount of exercise without overexertion.
- Joint Support Products: For older dogs, supplements like glucosamine and chondroitin can keep them active and moving comfortably.
4. Routine Veterinary Care Products
- Dental Chews and Brushes: Gum disease can exacerbate heart issues, so maintaining oral health is crucial.
Important Notes:
While these products can help support overall health, they cannot replace regular veterinary check-ups, a proper diet, and daily exercise. Always consult your veterinarian before introducing supplements, as they can recommend the best options for your dog’s unique needs.
Home Remedies
When it comes to Mitral Valve Disease (MVD), home remedies cannot cure or directly prevent the condition. However, certain lifestyle changes and natural practices can support your dog’s overall heart health and potentially slow the progression of the disease. That said, veterinary care remains essential for diagnosing and managing MVD. Here’s what you can do at home:
Home Remedies to Support Heart Health
1. A Balanced, Low-Sodium Diet
- Reducing sodium in your dog’s diet helps decrease fluid retention, easing strain on the heart. Opt for fresh, unseasoned foods (e.g., lean meats, vegetables) or vet-approved low-sodium diets.
- Avoid feeding processed dog foods or table scraps high in salt, such as chips or deli meats.
2. Heart-Healthy Supplements
- Fish Oil (Omega-3): Adds anti-inflammatory properties that benefit heart health.
- Hawthorn Berry (in vet-approved doses): A natural herb that may improve circulation and heart muscle strength. Always consult a veterinarian before using herbs.
3. Weight Control
- Maintaining a healthy weight reduces stress on your dog’s heart. Measure portions carefully and provide daily exercise tailored to your dog’s capabilities.
4. Gentle, Regular Exercise
- Daily walks or playtime help keep your dog’s heart active. Avoid overexertion, especially in breeds prone to heart issues or dogs already showing symptoms.
5. Stress Management
- Keep your dog’s environment calm and predictable to avoid unnecessary stress, which can elevate heart strain.
Why Vet Care Is Still Essential
- While these remedies may support heart health, MVD requires medical intervention to diagnose, monitor, and treat effectively. Medications like ACE inhibitors, diuretics, or beta-blockers are often necessary as the disease progresses. Additionally, vets can detect changes in your dog’s condition early through regular check-ups, which is key to managing MVD.
In Summary: Home remedies can complement professional care by improving your dog’s quality of life and slowing disease progression. However, they cannot replace a veterinarian’s expertise in preventing complications or providing life-saving treatments.
Action -call the vet
When to Call the Vet: Early Signs and Advanced Symptoms
Calling the veterinarian promptly when you suspect something is wrong with your dog can make all the difference in managing Mitral Valve Disease (MVD). Here’s how to know when it’s time to make that critical call, starting with early symptoms and moving into the more advanced stages.
How to Prepare for the Call
Whether you’re calling during the early stages or in an emergency, having key details ready can help your vet act quickly:
- Describe Symptoms Clearly: Include the timing, frequency, and severity of signs such as coughing, fatigue, or breathing difficulties.
- Note Activity Levels: Mention any recent changes in your dog’s behavior, like reduced energy or hesitancy to walk.
- Medication History: If your dog is already on heart medications or other treatments, provide a list of dosages and timing.
- Emergency Symptoms: Be specific about what you’ve noticed—e.g., “My dog collapsed while walking” or “They’re panting heavily without exertion.”
Questions to Ask Your Vet
When calling or visiting the vet, it’s important to ask questions to ensure you understand your dog’s condition and care plan. Some key questions include:
- What stage is my dog’s MVD, and what does that mean for treatment?
- What medications are recommended, and are there side effects?
- Should I monitor specific symptoms at home, and how often?
- Are there any lifestyle changes I should implement immediately?
- What are the next steps if symptoms worsen?
Having a list of questions prepared will help you feel confident about your dog’s treatment plan and ensure you don’t miss any crucial details.
Veterinary Treatment
Veterinary Treatment for Mitral Valve Disease
Treatment for Mitral Valve Disease (MVD) depends on how advanced the condition is at the time of diagnosis. Below is a breakdown of common treatments and veterinary actions based on the progression of the disease, including estimated 2024 costs where available.
Early-Stage Treatment: Managing Mild Symptoms
When MVD is caught early, the focus is on slowing the disease’s progression and managing mild symptoms.
- Diagnostic Tests
- Echocardiogram (Heart Ultrasound): To confirm the diagnosis and assess the condition of the heart.
- Estimated Cost: $400–$800.
- Chest X-rays: To evaluate the size of the heart and check for fluid buildup in the lungs.
- Estimated Cost: $150–$300.
- Bloodwork: To assess overall health and rule out concurrent conditions.
- Estimated Cost: $100–$200.
- Echocardiogram (Heart Ultrasound): To confirm the diagnosis and assess the condition of the heart.
- Medications
- ACE Inhibitors (e.g., Enalapril, Benazepril): These drugs help relax blood vessels, reducing the heart’s workload.
- Cost: $20–$40/month.
- Pimobendan (Vetmedin): Enhances heart contractility and reduces stress on the heart.
- Cost: $50–$150/month.
- ACE Inhibitors (e.g., Enalapril, Benazepril): These drugs help relax blood vessels, reducing the heart’s workload.
- Lifestyle Recommendations
- Adjust exercise routines to prevent overexertion.
- Begin monitoring symptoms at home to track any progression.
Middle-Stage Treatment: Symptom Management and Disease Control
At this point, symptoms like coughing, fatigue, and labored breathing become more evident. Treatment intensifies to manage symptoms and prevent complications like heart failure.
- Ongoing Diagnostics
- Frequent Echocardiograms or X-rays to monitor disease progression.
- Cost: $150–$500 per visit, depending on the complexity of testing.
- Frequent Echocardiograms or X-rays to monitor disease progression.
- Medications
- Diuretics (e.g., Furosemide): To reduce fluid buildup in the lungs or abdomen.
- Cost: $20–$40/month.
- Spironolactone: A potassium-sparing diuretic to complement Furosemide.
- Cost: $20–$50/month.
- Anti-Arrhythmics: To manage irregular heartbeats if detected.
- Cost: $30–$100/month.
- Diuretics (e.g., Furosemide): To reduce fluid buildup in the lungs or abdomen.
- Additional Support
- Dietary Changes: Prescription low-sodium diets to ease strain on the heart.
- Cost: $50–$100/month.
- Oxygen Therapy: At-home oxygen concentrators may be prescribed for advanced breathing difficulties.
- Cost: $300–$1,000 for the device, plus $50–$100/month for supplies.
- Dietary Changes: Prescription low-sodium diets to ease strain on the heart.
Late-Stage Treatment: Managing Severe Symptoms and Improving Comfort
In the advanced stages of MVD, treatment focuses on keeping the dog comfortable and addressing life-threatening symptoms.
- Emergency Stabilization
- If the dog experiences heart failure or severe respiratory distress, hospitalization may be required.
- Cost: $1,000–$3,000 for emergency care.
- If the dog experiences heart failure or severe respiratory distress, hospitalization may be required.
- Medications
- High doses of Diuretics to manage fluid buildup.
- Opiates (e.g., Butorphanol): To relieve severe respiratory distress or discomfort.
- Cost: $20–$50/dose.
- Palliative Care Options
- In some cases, the vet may recommend hospice care or discuss euthanasia if the dog’s quality of life is severely diminished.
- Euthanasia Cost: $100–$300 (at home or in clinic).
- In some cases, the vet may recommend hospice care or discuss euthanasia if the dog’s quality of life is severely diminished.
- Advanced Interventions
- For select cases, surgical valve repair or replacement is an emerging option at specialty clinics. However, this is highly invasive and expensive.
- Estimated Cost: $10,000–$20,000+ (limited availability in 2024).
- For select cases, surgical valve repair or replacement is an emerging option at specialty clinics. However, this is highly invasive and expensive.
Cost Overview for Each Stage
- Early-Stage Treatment: $70–$200/month for medications, plus diagnostic costs ($400–$1,000 upfront).
- Middle-Stage Treatment: $100–$300/month for medications and dietary adjustments, plus diagnostics ($150–$500 per visit).
- Late-Stage Treatment: $300–$1,000/month for medications and palliative care, plus emergency costs ($1,000–$3,000).
When to Expect Higher Costs
Costs increase significantly as the disease progresses due to the need for more frequent vet visits, advanced diagnostics, and emergency interventions. Being proactive with early diagnosis and treatment can reduce overall expenses and improve your dog’s quality of life.
Advancements in MVD Research
Veterinary medicine is constantly evolving, and exciting advancements are being made in the treatment of mitral valve disease. Emerging therapies include minimally invasive valve repair surgeries, innovative medications to optimize heart function, and regenerative stem cell treatments. Clinical trials are underway to explore new possibilities, giving hope to dogs with advanced cases of MVD. Speak to your veterinarian about cutting-edge options and whether your dog might benefit from these advancements.
Risk Factors

Risk Factors and Genetics in Mitral Valve Disease
Mitral Valve Disease (MVD) is influenced by several risk factors, some of which are preventable while others are inherent. Understanding these risks is crucial for dog owners and breeders in managing and reducing the prevalence of this condition.
Key Risk Factors
Obesity: Overweight dogs face increased strain on their heart, which accelerates the progression of MVD. Regular exercise and a balanced diet are essential in preventing obesity-related heart issues.
Genetics: Certain breeds are predisposed to MVD due to inherited traits. Cavalier King Charles Spaniels, for example, are notorious for their high prevalence of early-onset MVD.
Pre-existing Heart Conditions: Dogs with other heart-related ailments, such as valve degeneration or congenital defects, are at greater risk for developing MVD.
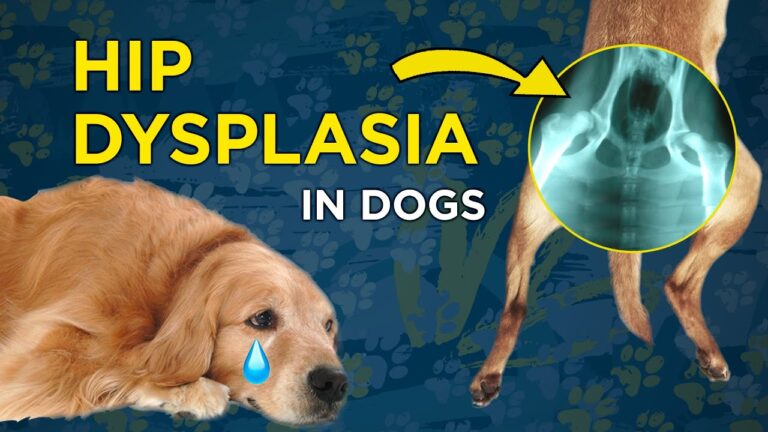
Genetic and Breed Considerations
Genetics plays a pivotal role in MVD. Small- to medium-sized breeds, such as the Cavalier King Charles Spaniel, Dachshund, and Chihuahua, have a higher incidence of the disease. In contrast, large and giant breeds, like the Great Dane or Irish Wolfhound, may also develop MVD but typically show symptoms later in life.
Responsible breeding is vital to reducing the prevalence of MVD. Ethical breeders perform health screenings on both parents before breeding, including echocardiograms to detect early signs of valve disease. By excluding affected dogs from breeding programs, the genetic pool is gradually improved, minimizing the transmission of this condition to future generations.
Breeders can also collaborate with veterinary cardiologists and participate in breed-specific registries to monitor health trends and implement better breeding standards. Education and transparency about potential genetic risks are essential for both breeders and prospective dog owners.
Common Misconceptions
“MVD Only Affects Old Dogs”: While age is a factor, certain breeds can develop symptoms at a young age due to genetic predisposition.
“If My Dog Looks Healthy, It’s Fine”: MVD can progress silently in its early stages, making routine heart check-ups critical for at-risk breeds.
“Breeding Two Healthy-Looking Dogs Ensures Healthy Puppies”: Without genetic testing, even healthy-appearing dogs can pass on the risk of MVD.
By understanding these risk factors and encouraging responsible breeding practices, we can work toward reducing the impact of MVD on future generations. Owners can also do their part by maintaining their dog’s weight, scheduling regular veterinary check-ups, and staying informed about the unique health needs of their breed.
Psychological Factors
Psychological Factors in Managing Mitral Valve Disease: The Impact of Stress and the Power of a Calm Environment
Mitral Valve Disease (MVD) is not just a physical condition—it can significantly affect a dog’s mental well-being. Stress and anxiety can exacerbate symptoms, making management more challenging for both dogs and their owners. Creating a calm, stress-free environment is vital in improving a dog’s quality of life and ensuring a smoother progression of the disease.
The Link Between Stress and MVD Symptoms
When a dog experiences stress or anxiety, their body releases hormones like cortisol and adrenaline, which can elevate heart rate and blood pressure. For dogs with MVD, these physiological changes can strain their already compromised heart, potentially triggering or worsening symptoms like coughing, labored breathing, or fatigue. Prolonged stress may even accelerate the progression of the disease by increasing the heart’s workload over time.
Dogs with MVD may become anxious due to physical discomfort or changes in their daily routines caused by the disease. For example, the inability to engage in favorite activities, like long walks or playful romps, may cause frustration or depression. Additionally, if their owner is visibly stressed about their condition, dogs can sense and mirror this anxiety, creating a feedback loop that further impacts their health.
Creating a Calm Environment
A calm and reassuring environment can do wonders for dogs with MVD. Here are some ways to help them feel secure and relaxed:
Maintain a Routine: Consistency is key for dogs with heart disease. Feeding, medication, and light exercise schedules should be regular to reduce anxiety.
Comfortable Living Spaces: Provide a quiet, cozy area for rest, away from loud noises or disturbances. Orthopedic beds and soft blankets can offer additional comfort. If they use a crate to sleep in a simple blanket over the crate to make a “Cave” goes a long way to making them feel safe and comfortable.
Use Calming Aids: Products like pheromone diffusers, calming sprays, or anxiety wraps (e.g., Thunder Shirts) can help reduce stress. Some dogs may also benefit from natural supplements like chamomile or valerian root but always consult your vet before introducing new products.
Positive Reinforcement: Reward calm behavior with gentle praise or treats. This helps your dog associate relaxation with positive outcomes.
The Role of Light Activity and Gentle Interaction
Physical activity must be carefully moderated, but light, calm exercise can be beneficial for both mental and physical health. Short, slow-paced walks or gentle indoor games like scent work can engage your dog’s mind without straining their heart.
Interactive toys or puzzle feeders can also provide mental stimulation, keeping your dog entertained and reducing boredom-induced stress. Be cautious to avoid overly stimulating activities, as excitement can also elevate heart rate.
Owner Stress and Its Impact
As a dog owner, your emotional state has a direct influence on your pet’s well-being. Dogs are highly attuned to their humans and can pick up on stress or worry. Taking care of your own mental health is an essential part of supporting a dog with MVD. Practices like mindfulness, deep breathing, or even seeking support from pet-owner communities can help you stay calm and focused.
The Positive Power of a Stress-Free Environment
When stress is minimized, dogs with MVD are better able to conserve energy, enjoy daily activities, and respond positively to treatment plans. A calm dog is less likely to experience exacerbated symptoms like rapid breathing or coughing, allowing their heart to function as efficiently as possible despite the disease.
By focusing on reducing stress and providing a stable, peaceful environment, you can make a significant difference in your dog’s quality of life. Remember, a happy and calm pet is not only more comfortable but also more likely to enjoy the time they have with you, no matter the challenges of living with MVD.
Surgical Options
Surgical Options for Mitral Valve Disease: When Is It Necessary?
When Mitral Valve Disease (MVD) progresses to an advanced stage where medical management alone no longer controls symptoms, surgical intervention may be necessary. Surgery is often considered when a dog’s quality of life is severely impacted, or when heart failure caused by MVD becomes life-threatening. The decision to proceed with surgery is made after comprehensive diagnostics, including echocardiograms, X-rays, and consultations with a veterinary cardiologist.
Types of Surgical Procedures for MVD
The most common surgical approach for MVD in dogs is mitral valve repair. This delicate procedure involves reconstructing the mitral valve to improve its functionality, prevent regurgitation of blood, and restore normal blood flow through the heart. Another less common option is mitral valve replacement, where a prosthetic valve is implanted to replace the damaged valve.
Mitral valve repair is generally preferred over replacement due to lower risks of complications and a higher success rate in dogs.
Success Rates and Outcomes
Mitral valve surgery has shown promising results, with a reported success rate of approximately 85-90% in dogs when performed by experienced veterinary surgeons. Dogs that undergo successful surgery often experience a significant improvement in their quality of life, with a reduction or elimination of symptoms such as coughing, fatigue, and difficulty breathing.
However, the success of the surgery depends on various factors, including the dog’s overall health, the stage of the disease, and whether there are additional complications such as arrhythmias or pulmonary hypertension.
Post-Surgical Recovery and Care
Recovery from mitral valve surgery requires diligent post-operative care. Dogs typically spend several days in an intensive care unit (ICU) for close monitoring by veterinary specialists. During this time, their heart function, blood pressure, and oxygen levels are continuously assessed to detect and manage any complications early.
Once discharged, the recovery period at home can last several weeks. Owners play a critical role in ensuring a smooth recovery by adhering to the following care guidelines:
Restricted Activity: Dogs must avoid strenuous activity or excitement during the recovery period to prevent strain on the healing heart. Short, controlled leash walks are usually allowed.
Medications: Post-surgical medication may include pain relievers, antibiotics to prevent infection, and diuretics or ACE inhibitors to support heart function.
Dietary Management: A low-sodium diet may be recommended to minimize fluid retention and reduce the workload on the heart.
Follow-Up Appointments: Regular check-ups with the veterinary cardiologist are essential to monitor the heart’s healing process and overall health.
With proper care, many dogs can return to a near-normal lifestyle and enjoy several additional years of good quality life after surgery.
2024 Financial numbers of cost.
The cost of mitral valve surgery and follow-up care for dogs with Mitral Valve Disease (MVD) can vary depending on several factors, such as the location, the expertise of the veterinary surgeon, and the specific needs of the dog. Here’s a breakdown of typical costs:
Surgery Costs
Mitral Valve Repair Surgery: The surgery itself generally costs between $15,000 and $30,000, depending on the veterinary facility and the complexity of the procedure. This cost often includes pre-surgical testing, anesthesia, the surgery, and the initial ICU stay for post-operative monitoring.
Additional Fees: There may be extra charges for unforeseen complications, extended ICU care, or specialized diagnostics, which could add another $1,000 to $5,000.
Follow-Up Costs
Post-surgical care and follow-ups can also be significant but are typically more manageable than the surgery itself. Here are some common expenses:
Medications:
Pain relievers: $30–$100 per month.
Antibiotics (if prescribed): $20–$50 per course.
Heart medications (e.g., ACE inhibitors, diuretics): $50–$200 per month, depending on the dosage and specific drugs.
Follow-Up Appointments:
Routine cardiology check-ups: $300–$800 per visit, depending on the diagnostic tests performed (e.g., echocardiograms, X-rays).
Frequency: These visits are usually required every 3 to 6 months, but this may vary based on the dog’s recovery.
Dietary Adjustments:
Specialized low-sodium diets: $50–$100 per month, depending on the brand and size of your dog.
Rehabilitation (if needed):
Physical therapy sessions (if recommended): $50–$100 per session.
Lifetime Costs
When considering the costs of surgery, post-surgical care, and long-term management, owners can expect to spend between $20,000 and $50,000 over the course of their dog’s treatment. For dogs that are managed medically without surgery, lifetime costs for medications, diagnostics, and routine care typically range from $5,000 to $15,000, depending on the severity of the condition and lifespan.
Financial Assistance Options
Due to the high cost of mitral valve surgery, some pet owners consider:
Pet Insurance: Ensure coverage includes congenital or chronic conditions if purchased early.
Payment Plans: Many specialty hospitals offer payment plans or financing options, such as CareCredit.
Charitable Organizations: Some nonprofit organizations provide financial assistance for lifesaving veterinary treatments.
It’s important to consult with your veterinarian or veterinary cardiologist to discuss a tailored plan for your dog’s care and understand the specific costs in your region.
Monitoring
Monitoring Symptoms and Follow-Up Care for MVD
Whether your dog has undergone surgery or is being managed medically, ongoing monitoring is crucial to track symptoms and ensure timely intervention if the disease progresses.
Why Monitoring Is Important
Mitral Valve Disease is a chronic condition that can worsen over time. Early detection of changes in your dog’s symptoms allows your veterinarian to adjust treatment plans and improve outcomes. Monitoring also helps ensure that complications such as fluid buildup in the lungs or irregular heart rhythms are promptly addressed.
Tracking Symptoms at Home
Owners are an essential part of the monitoring process. Here are some key symptoms to track and report to your veterinarian:
Coughing: Keep note of the frequency, severity, and time of day your dog coughs. A worsening cough may indicate fluid accumulation or worsening valve function.
Breathing Difficulties: Watch for signs such as labored or rapid breathing, particularly during rest or sleep.
Activity Levels: Monitor your dog’s tolerance for exercise and play. A noticeable decrease in energy or reluctance to move could be a red flag.
Appetite and Weight: Changes in appetite or unexplained weight loss can signal advanced disease.
Behavioral Changes: Increased anxiety, restlessness, or trouble sleeping may also indicate disease progression.
Use a journal or a mobile app to record these observations regularly, as detailed notes will be invaluable for your veterinarian during follow-up visits.
Follow-Up Appointments
Regular veterinary check-ups are vital for dogs with MVD, whether or not they have had surgery. These visits typically include:
Physical Exams: Your vet will listen to your dog’s heart and lungs for changes in heart murmurs or abnormal sounds.
Diagnostic Tests: Echocardiograms, chest X-rays, or blood tests may be repeated periodically to assess heart function and detect fluid buildup.
Treatment Adjustments: Based on the findings, your vet may modify medications, recommend dietary changes, or suggest additional treatments.
A Team Effort for Your Dog’s Heart Health
Mitral Valve Disease requires a proactive and collaborative approach between you and your veterinary team. By understanding when surgery is necessary, providing attentive post-surgical care, and staying vigilant with monitoring, you can help your dog lead a healthier, happier life. Regular communication with your vet and a commitment to your dog’s well-being are the cornerstones of managing this condition effectively.
Quality of Life Considerations
A dog’s quality of life should always be a priority, especially when managing a chronic condition like MVD. Assess your pet’s comfort regularly—are they able to eat, sleep, and move comfortably? Symptoms like frequent coughing or difficulty breathing can impact their happiness. Work closely with your vet to manage symptoms and adjust treatment plans as needed. Small changes, such as providing orthopedic bedding or keeping your dog in a temperature-controlled environment, can significantly enhance their comfort and overall well-being.
Living with a Dog with MVD
Living with a dog diagnosed with mitral valve disease requires thoughtful adjustments to your routine. Dogs with MVD may need modified exercise, a low-sodium diet, and frequent vet checkups. Maintaining a calm, stress-free environment is critical, as stress can exacerbate heart issues. Owners should monitor breathing patterns, note changes in energy levels, and provide a comfortable space for rest. With the right care, many dogs with MVD can continue to enjoy happy, active lives.
Emergency Contacts
Emergency Contacts: Recognizing When to Act Fast for Mitral Valve Disease
When to Seek Emergency Care: Key Warning Signs
In cases of Mitral Valve Disease (MVD), recognizing the signs of a medical emergency is critical to your dog’s survival. While early symptoms like coughing or fatigue warrant a vet appointment, certain symptoms demand immediate action. Severe breathing distress is one of the most urgent red flags. If your dog is gasping for air, struggling to breathe, or you notice a bluish tint on the gums or tongue, this indicates oxygen deprivation and requires immediate veterinary care. Similarly, fainting or collapse—often referred to as syncope—could mean the heart is struggling to maintain adequate blood flow. Lastly, if your dog becomes unresponsive or lethargic to the point of immobility, it is a life-threatening situation that needs emergency attention.
While these symptoms are directly associated with advanced MVD, they can also be mistaken for other medical conditions such as respiratory infections or heatstroke. However, any such symptoms should always be treated as emergencies regardless of the underlying cause. Waiting to see if symptoms improve could mean the difference between life and death.
Preparedness Tips for Emergencies
Being prepared can reduce the stress of an emergency and save precious time. Start by keeping a list of 24/7 emergency veterinary clinics within driving distance. Save these contacts on your phone and post them in a visible spot at home, such as your refrigerator. Many clinics also offer telehealth services for initial guidance—having their apps or numbers readily available can be invaluable.
Another critical step is preparing a “go bag” for emergency vet visits. This bag should include your dog’s medical records, a list of current medications, a recent photo of your dog for identification, and essential supplies like a leash, muzzle, and comfort items such as a blanket. If your dog has dietary restrictions, include a small portion of their specialized food to sustain them during extended hospital stays.
Practice loading your dog into the car quickly, especially if they are a large or giant breed, as logistics can become complicated during a panic. Additionally, ensure that any caregivers or family members know how to recognize emergency symptoms and where the “go bag” is stored.
By acting swiftly, recognizing emergency signs, and being prepared, you can maximize your dog’s chances of recovery and ensure they receive the critical care they need.