What Is Dental Disease in Dogs?
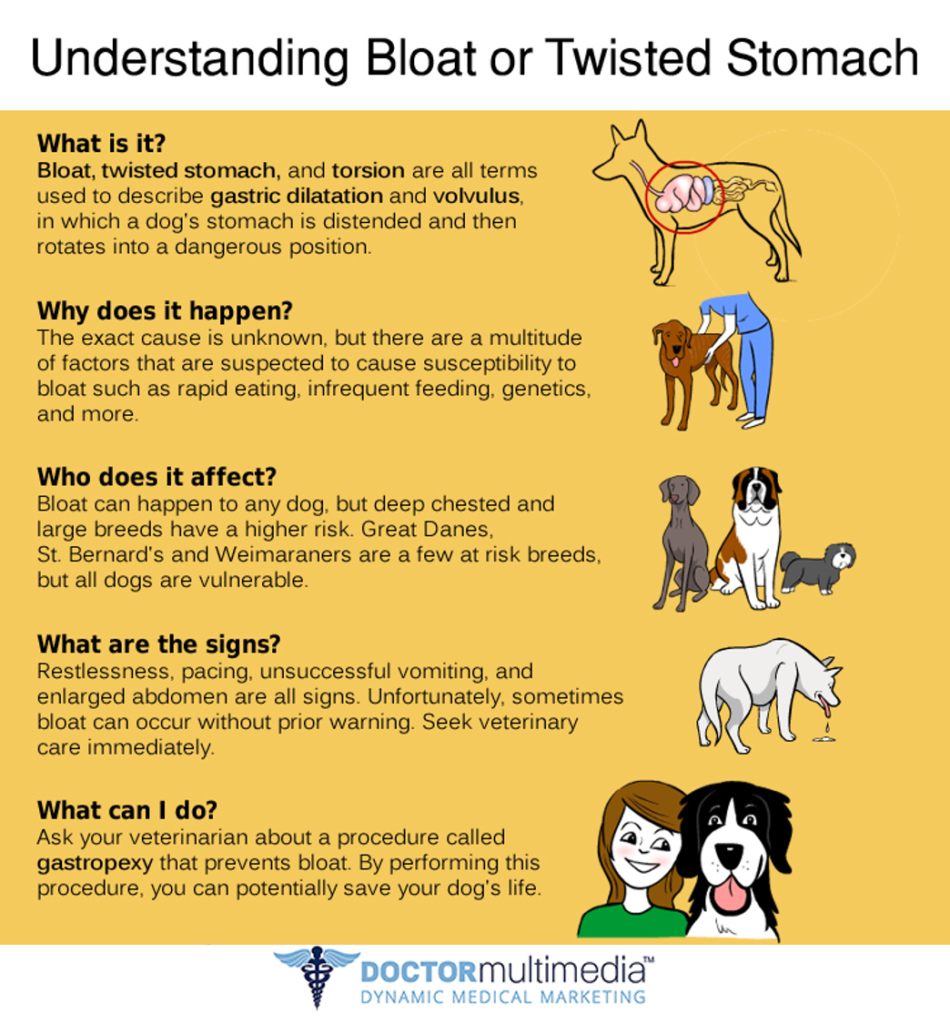
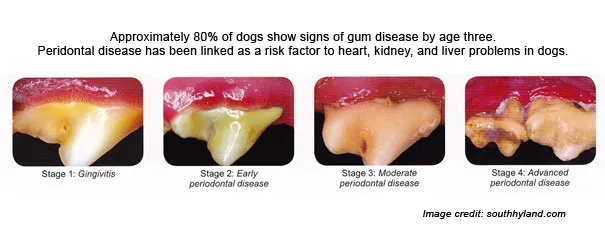
Dental disease in dogs, also called periodontal disease, is one of the most common health issues, affecting an estimated 80% of dogs by the age of three. It involves conditions that impact the teeth, gums, and structures that support the teeth. These conditions can range from mild gum inflammation (gingivitis) to severe damage to the bones and ligaments that hold the teeth in place (periodontitis). In advanced stages, dental disease can affect not only the mouth but also a dog’s overall health, potentially leading to infections in vital organs such as the heart, liver, and kidneys.
Common Symptoms of Dental Disease
Owners can often detect dental disease early by observing their dog’s behavior and inspecting their mouth regularly. Here are the most common symptoms:
1. Bad Breath (Halitosis):
While some level of bad breath can be normal for dogs, persistent foul-smelling breath is often the first sign of dental disease. It’s caused by the buildup of bacteria in the mouth, especially from tartar and plaque on the teeth. See Halitosis Breath below for a clarification.
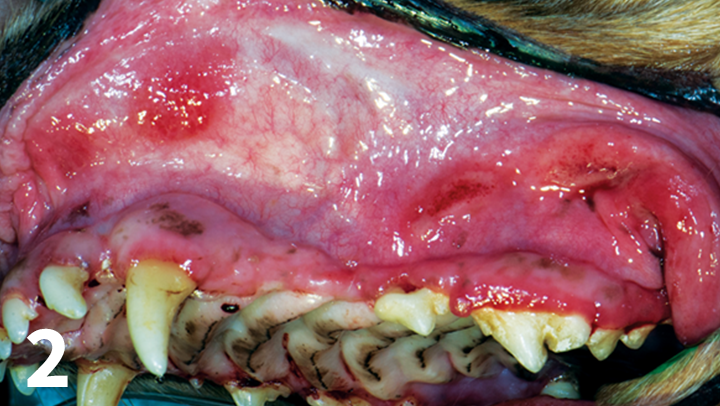
2. Red, Swollen, or Bleeding Gums:
Gingivitis, an early form of gum disease, can cause the gums to appear red and swollen. They may also bleed when the dog chews on toys or during brushing.
3. Plaque and Tartar Buildup:
Plaque is a sticky film of bacteria that forms on the teeth. If not cleaned away, it hardens into tartar, which appears as a yellow or brown layer on the teeth, especially near the gumline.
4. Excessive Drooling:
Dogs with dental disease may drool more than usual, and their saliva may appear stringy or tinged with blood.
5. Difficulty Chewing or Eating:
If a dog hesitates before eating, drops food from its mouth, or chews on only one side of the mouth, it could be a sign of oral pain. Dogs with severe dental disease may avoid hard foods like kibble or treats, preferring softer foods instead.
6. Loose or Missing Teeth:
Advanced dental disease can cause teeth to become loose or even fall out due to bone and tissue loss. If teeth appear crooked or displaced, it’s a sign that they may be loose.
7. Pawing at the Mouth or Face:
Dogs in pain may paw at their mouth or face, especially if they have toothaches or abscesses.
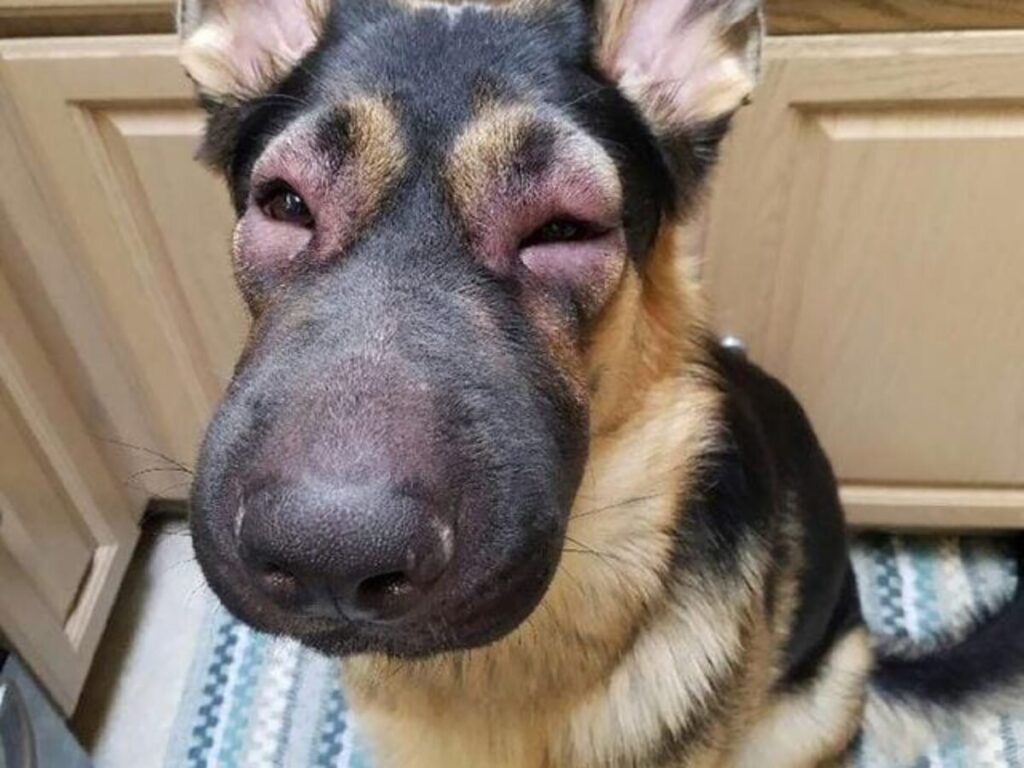
8. Swelling Around the Mouth or Jaw:
Oral infections, such as tooth abscesses, can cause noticeable swelling around the mouth, face, or jaw. This is a more advanced symptom of dental disease that requires immediate veterinary care.
9. Behavioral Changes:
Dogs with dental pain may become more irritable or withdrawn. They might avoid play or appear lethargic and less interested in activities they usually enjoy.
10. Discolored Teeth or Gums:
Teeth affected by dental disease may appear yellow, brown, or even gray, while the gums may look dark red or purple.
Types of Dental Disease in Dogs
There are several types of dental disease that affect dogs, each with varying levels of severity. These are the most common:
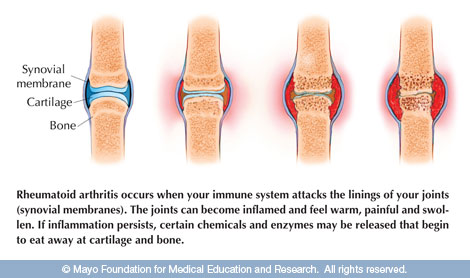
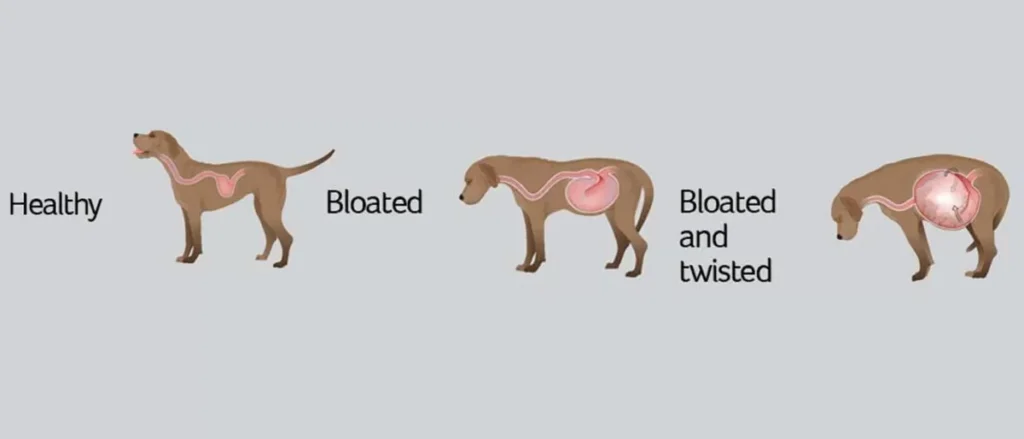
1. Gingivitis:
Gingivitis is the early stage of periodontal disease, characterized by inflammation of the gums caused by the accumulation of plaque. If caught early, gingivitis can be reversed through proper dental care, including brushing, dental cleanings, and possibly antibiotics.

2. Periodontitis:
When gingivitis progresses untreated, it leads to periodontitis, a more severe form of dental disease. In periodontitis, the inflammation spreads to the deeper structures supporting the teeth, such as the bones and ligaments. This can lead to gum recession, bone loss, and eventually tooth loss.

3. Tooth Abscesses:
A tooth abscess occurs when a bacterial infection forms at the root of a tooth, leading to a pocket of pus. Abscesses are very painful and can cause swelling in the face or jaw. In most cases, tooth extraction and antibiotics are necessary to treat the infection.

4. Tooth Fractures:
Dogs that chew on hard objects, such as bones, antlers, or ice, can fracture their teeth. Some tooth fractures may expose the tooth’s sensitive pulp, leading to infections and pain. Treatment for tooth fractures may include root canals or extractions.

5. Tartar/Calculus Buildup:
When plaque hardens into tartar (also called calculus), it adheres to the teeth and is difficult to remove without professional dental cleaning. Tartar can irritate the gums and lead to gum disease.
6. Stomatitis:
Stomatitis is a condition in which the mucous membranes inside the mouth become inflamed. This inflammation can extend to the gums, tongue, and inner cheeks. It’s often painful and can make eating difficult for dogs.
7. Oral Tumors:
While less common, oral tumors can occur in dogs, affecting the gums, tongue, or other parts of the mouth. Tumors can be benign (non-cancerous) or malignant (cancerous), and any suspicious growths in the mouth should be evaluated by a veterinarian.

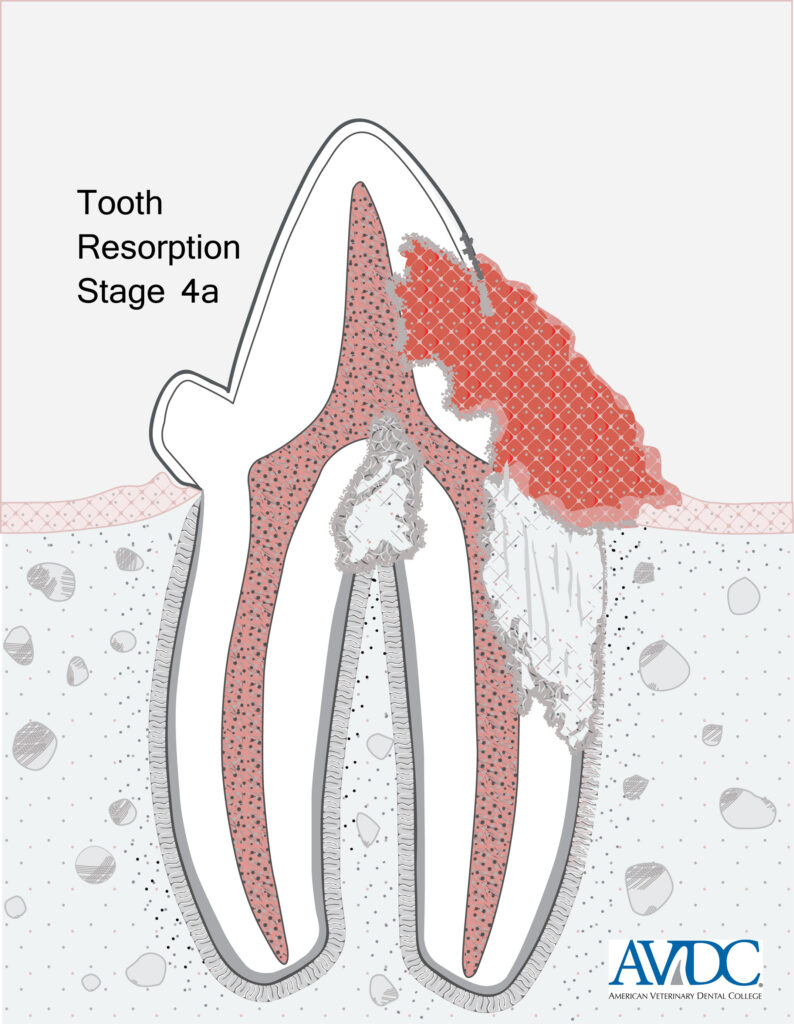
8. Resorptive Lesions:
These lesions occur when the body begins to break down the structure of the tooth, usually at the gumline. This condition is very painful and often requires extraction of the affected tooth.
9. Malocclusion:
Malocclusion refers to misalignment of the teeth, which can cause uneven wear, difficulty chewing, and an increased risk of dental disease.

10. Oral Infections:
Infections can develop in the mouth due to injuries, foreign objects, or untreated dental disease. These infections can cause swelling, pain, and pus discharge.

Conclusion
Dental disease in dogs is a common and potentially serious health issue that affects not only the mouth but the overall well-being of the dog. Recognizing the early symptoms, such as bad breath, red gums, and difficulty eating, can help owners seek veterinary care before the condition worsens. There are many types of dental disease, ranging from reversible gingivitis to severe periodontitis and abscesses. With proper dental care, including daily brushing, regular vet visits, and professional cleanings, owners can help prevent the progression of dental disease and ensure their dog leads a pain-free and healthy life.
Halitosis Breath
How can I tell the difference between dog breath and signs of dental disease
Dogs often have naturally foul-smelling breath from their typical behaviors, like licking themselves or eating things they shouldn’t. However, there are key differences between “normal” dog breath and the bad breath (halitosis) that indicates dental disease. Here’s how to tell:
1. Consistency and Persistence:
– Normal dog breath: Occasional bad breath that goes away after a while is usually due to something the dog recently ate or licked.
– Dental disease-related bad breath: If the foul odor is persistent and doesn’t improve even after brushing or changing food, it’s likely due to plaque buildup, gum infection, or tooth decay.
2. Intensity:
– Normal dog breath: The smell is usually unpleasant but mild.
– Dental disease-related bad breath: Halitosis from dental disease tends to be much stronger, more offensive, and has a sour or rotten odor that’s hard to ignore.
3. Accompanied by Other Symptoms:
– Dental disease often comes with additional symptoms like:
– Red or swollen gums
– Drooling more than usual
– Reluctance to chew or eat
– Pawing at the mouth
– If you notice any of these along with bad breath, it’s a sign that there may be a more serious dental issue.
4. Food and Behavior History:
– If your dog’s bad breath coincides with eating something they shouldn’t (like garbage or feces), it may pass within a day or two. But if the bad breath persists over time, it’s worth investigating further.
By observing the breath’s consistency, intensity, and whether it’s linked to other symptoms, you’ll be better able to distinguish between “doggy breath” and a dental issue that needs vet attention.
Prevention
Preventing dental disease in dogs is crucial for their overall health and well-being. Here are some effective steps that owners can take to reduce the risk of dental issues:
1. Daily Brushing:
One of the most effective ways to prevent dental disease is by brushing your dog’s teeth daily. Use a toothbrush and toothpaste specifically designed for dogs, as human toothpaste can be harmful. Brushing helps remove plaque before it hardens into tartar, which can lead to gum disease.
2. Dental Chews and Toys:
Providing your dog with dental chews and toys can help reduce plaque buildup. These products are designed to scrape off tartar as the dog chews, while also satisfying their natural urge to chew. Look for dental chews approved by the Veterinary Oral Health Council (VOHC) for added effectiveness.
3. Regular Vet Checkups and Professional Cleanings:
Routine veterinary checkups should include dental assessments to catch any early signs of dental disease. Vets can perform professional cleanings under anesthesia to thoroughly remove tartar and plaque that can’t be reached with at-home care. Most dogs benefit from a professional cleaning once a year, especially as they age.
4. Special Dental Diets:
Some commercial dog foods and treats are designed to promote oral health by reducing tartar buildup. These diets have a unique texture or ingredients that help clean the teeth as the dog chews.
5. Water Additives and Oral Rinses:
Water additives and oral rinses can help control bacteria in the mouth and prevent plaque buildup. These products are easy to use, as they can be added to your dog’s water or applied directly to their gums.
By incorporating these preventive measures into your dog’s routine, you can significantly reduce the risk of dental disease and keep their mouth healthy.
Products to Help
Here is a list of popular products on Amazon that can help prevent dental disease in dogs:
1. Virbac C.E.T. Enzymatic Toothpaste
– This dog-specific toothpaste contains enzymes to help break down plaque and prevent tartar buildup. It’s available in flavors that appeal to dogs, making brushing easier.
2. Vet’s Best Enzymatic Dog Toothpaste & Toothbrush Kit
– This complete kit includes a toothpaste with aloe, neem oil, and enzymes, along with a dual-ended toothbrush for cleaning teeth at different angles.
3. Greenies Dental Chews
– These are popular dental treats that help clean teeth and freshen breath as dogs chew them. They are VOHC-approved and available in different sizes.
4. Arm & Hammer for Pets Dental Spray
– This spray helps control tartar and plaque without the need for brushing. It is a simple solution for dogs that resist brushing.
5. Dental Fresh Water Additive
– A water additive that helps freshen breath and prevent plaque buildup. Simply add it to your dog’s water bowl daily.
6. Virbac C.E.T. VeggieDent Chews
– These plant-based chews are another VOHC-approved product that helps reduce tartar and promote fresh breath.
7. Petrodex Finger Toothbrush
– A rubber toothbrush that fits on your finger, allowing for better control when cleaning your dog’s teeth.
8. TropiClean Fresh Breath Oral Care Gel
– A gel that can be applied directly to the gums and teeth to help reduce tartar and freshen breath.
By incorporating these products into your dog’s dental care routine, you can significantly reduce the risk of dental disease and keep their mouth healthy.
When to Take Your Dog to the Vet
When dental prevention measures aren’t employed or fail, it’s crucial for owners to recognize the signs of dental disease early and seek veterinary care. Here’s when it’s time to take your dog to the vet and what actions the vet would typically take:
You should take your dog to the vet if you notice any of the following signs of dental disease:
1. Bad Breath (Halitosis): Persistent foul-smelling breath is one of the earliest indicators of dental disease, especially if it’s more pronounced than normal dog breath.
2. Visible Plaque or Tartar: Yellow or brown buildup on the teeth, particularly around the gum line, is a sign of plaque hardening into tartar, which can lead to infection and inflammation.
3. Swollen or Bleeding Gums: Inflamed, red, or bleeding gums (a sign of gingivitis) indicate early-stage periodontal disease.
4. Reluctance to Eat: If your dog is reluctant to eat hard foods or shows signs of discomfort when chewing, it could be due to dental pain.
5. Loose or Missing Teeth: If teeth appear to be loose or if your dog has missing teeth, this indicates advanced periodontal disease that requires immediate attention.
6. Excessive Drooling: Excessive drooling or pawing at the mouth could be a sign of oral pain or infection.
7. Pus or Swelling in the Mouth: If there’s pus around the gums or swelling in the face, it may be an abscess or severe infection requiring urgent care.
Veterinary Treatment
What Actions the Vet Will Take
When you bring your dog to the vet for dental concerns, they will perform a comprehensive examination and recommend appropriate treatments based on the severity of the condition. Here’s what to expect:
1. Physical Examination:
– The vet will begin with a visual examination of your dog’s mouth, checking for signs of tartar buildup, gum disease, loose teeth, and infection. They will also assess your dog’s overall health to ensure that it is safe for dental procedures under anesthesia.
2. Dental Cleaning:
– If the vet determines that dental disease is present, they will likely recommend a professional dental cleaning. This is performed under general anesthesia to allow the vet to thoroughly clean and treat the teeth. During the cleaning:
– Scaling: Tartar is removed from the surface of the teeth using both manual tools and ultrasonic scalers.
– Polishing: The teeth are polished to smooth the enamel and make it more difficult for plaque to reattach.
– Gum Treatment: If there is gingivitis or early-stage periodontal disease, the vet will treat the gums to reduce inflammation and infection.
3. Dental X-rays:
– In many cases, the vet will take dental x-rays to assess the health of the tooth roots and jawbone, as dental disease often progresses below the gum line.
4. Extractions:
– If a tooth is severely damaged or infected, the vet may recommend extraction. Tooth extractions are common in advanced dental disease and help prevent the spread of infection.
5. Medication:
– The vet may prescribe antibiotics if there is an infection present in the mouth. Pain medication may also be given if extractions or other invasive procedures were performed.
6. Follow-up and Maintenance:
– After treatment, the vet will discuss at-home care and prevention strategies to maintain oral health, which may include regular brushing, dental chews, and follow-up cleanings as needed.
By addressing dental disease early with professional veterinary care, you can prevent more severe complications like abscesses, tooth loss, and systemic infections that can affect your dog’s overall health.
Home Remedies
Holistic home remedies can play a supportive role in managing and treating early-stage dental disease in dogs. While these remedies are not a substitute for professional veterinary care, they can help maintain oral health and reduce the progression of dental issues. Here are a few holistic approaches that owners can try:
1. Coconut Oil
Coconut oil has natural antibacterial properties and can help reduce plaque buildup in dogs. Owners can apply a small amount of coconut oil to their dog’s gums and teeth or mix it with their food. The oil can also be used as a base for brushing, as it helps kill harmful bacteria in the mouth and freshens breath.
2. Raw Bones (Under Supervision)
Raw bones, particularly beef knuckle bones, can help naturally scrape plaque off a dog’s teeth while they chew. The texture of the bone acts as a natural toothbrush. However, it’s essential to use raw bones and not cooked ones, as cooked bones can splinter and cause injury. Always supervise your dog when giving them bones.
3. Apple Cider Vinegar
Adding a small amount of apple cider vinegar (about a teaspoon) to your dog’s water bowl can help maintain oral hygiene. Apple cider vinegar is known for its antibacterial properties, which can reduce bacteria in the mouth, helping to prevent plaque buildup and reduce bad breath.
4. Aloe Vera Gel
Aloe vera gel can soothe inflamed gums and may help with mild gum disease. Apply a small amount of natural aloe vera gel to your dog’s gums with your finger or a soft cloth. Make sure to use an organic, dog-safe product without additives.
5. Herbal Rinses
Some herbs, such as parsley and mint, can freshen breath and help control bacteria. You can make a simple herbal rinse by steeping fresh parsley in boiling water, letting it cool, and then applying it to your dog’s gums with a soft cloth or adding it to their water bowl.
While these remedies can help reduce the risk of dental disease, they should complement—not replace—regular dental checkups and professional cleanings from your vet.
Risk Factors for Dental Disease in Dogs
Dental disease in dogs is a multifaceted health issue influenced by various risk factors, including breed, genetics, lifestyle, diet, and even psychological factors. Understanding these risks can help dog owners take proactive steps to prevent or manage the onset of dental problems.
1. Age
One of the most significant risk factors for dental disease is age. As dogs get older, they are more likely to develop dental issues such as periodontal disease. By the age of three, most dogs show some signs of dental disease, and the risk increases with age.
2. Diet
Diet plays a crucial role in dental health. Dogs that eat primarily soft or wet food are more likely to develop plaque and tartar than those that consume dry kibble, which can help scrape the teeth. Additionally, dogs that are fed human food or sugary treats are at a higher risk of dental problems.
3. Lack of Dental Care
Dogs that do not receive regular dental care—such as tooth brushing, dental chews, or professional cleanings—are at a higher risk of developing dental disease. Plaque can quickly harden into tartar, leading to gum inflammation, infection, and tooth loss if not managed properly.
4. Poor Oral Hygiene
Poor oral hygiene, whether due to lack of brushing or neglect in professional dental care, allows bacteria to thrive in the dog’s mouth. This bacteria leads to plaque formation, which can calcify into tartar and eventually cause gum disease and tooth decay.
5. Chewing Habits
Some dogs have destructive chewing habits, like chewing on hard objects (bones, sticks, rocks) that can damage their teeth. Tooth fractures are a common result of aggressive chewing, leading to pain, infection, and further dental complications.
Genetic and Breed Considerations
Genetics and breed play a role in dental health. Some breeds are more predisposed to dental issues than others, particularly smaller breeds and specific giant breeds.
1. Toy and Small Breeds
Small dog breeds like Chihuahuas, Yorkshire Terriers, and Pomeranians are particularly prone to dental disease. These dogs often have overcrowded teeth in their small mouths, making it easier for plaque and tartar to build up in tight spaces. Additionally, smaller dogs tend to live longer, and thus, their teeth undergo more wear and tear over time.
2. Giant Breeds
In giant breeds like Great Danes, Mastiffs, and Saint Bernard‘s, dental issues may stem from the size of the teeth and jaw alignment. These dogs can be prone to misaligned teeth, which can cause uneven wear and tear and lead to periodontal disease. While large breeds are not as prone to overcrowding like smaller dogs, they still require regular dental care to prevent disease.
3. Brachycephalic Breeds
Breeds with short muzzles, like Bulldogs, Boxers, and Pugs, are also at higher risk for dental problems due to the structure of their mouths. These breeds often have misaligned or crowded teeth, making it harder for owners to clean properly and leading to a higher risk of plaque buildup.
4. Genetic Predisposition
Some dogs are genetically predisposed to poor dental health. For example, certain breeds may have weaker enamel, making them more prone to cavities or tooth fractures. Others may have hereditary issues with their gums, such as chronic gingivitis, which can quickly progress into periodontal disease if not managed.
Psychological Factors and Dental Disease
Interestingly, psychological factors can also contribute to dental disease in dogs. While not as widely discussed, stress, anxiety, and certain behaviors can impact a dog’s oral health in the following ways:
1. Stress and Anxiety
Stress and anxiety can lead to behaviors that negatively affect a dog’s dental health. For example, dogs with separation anxiety may engage in destructive chewing behaviors, which can result in cracked or broken teeth. Additionally, stress can weaken the immune system, making it harder for the body to fight off oral infections.
2. Behavioral Issues
Some dogs that suffer from anxiety or boredom may excessively chew on inappropriate objects like rocks, metal, or furniture. These hard objects can chip or fracture teeth, leading to pain, infections, and the need for extractions.
3. Reluctance to Eat
Dogs with dental pain may be reluctant to eat, especially hard kibble, leading to nutritional deficiencies that can further worsen their health. Psychological stress from pain can also cause behavioral changes, making it harder for owners to detect the underlying dental issue.
4. Resistance to Dental Care
Dogs that are fearful or anxious may resist routine dental care, such as tooth brushing or oral exams. This resistance can make it challenging for owners to provide proper dental hygiene, allowing plaque and tartar to build up unchecked.
Conclusion
Dental disease in dogs is influenced by a range of risk factors, including age, diet, lack of care, and genetic predisposition. While certain breeds are more prone to dental issues due to their size or mouth structure, all dogs require regular dental care to maintain oral health. Psychological factors, such as stress and destructive chewing, can also contribute to dental problems, underscoring the importance of both physical and mental well-being for dogs.
Preventative care, including regular brushing, dental chews, and professional cleanings, is essential for maintaining a dog’s oral health. Early detection of dental disease can prevent more severe complications, such as tooth loss, infections, and systemic health issues. As part of a comprehensive health care plan, addressing both the physical and psychological factors that contribute to dental disease will help ensure that dogs lead healthier, happier lives.
Surgical Options for Dental Disease in Dogs
When dental disease in dogs progresses to more advanced stages, surgery may be necessary to address the underlying issues. Here are the most common surgical treatments:
1. Tooth Extractions
One of the most common surgical procedures for severe dental disease is tooth extraction. If a tooth is badly decayed, fractured, or causing a significant infection (abscess), extraction is often the best option. This helps prevent further complications, such as the spread of infection to the jawbone or other teeth.
– Cost: Extractions can range from $500 to $1,000 or more per tooth, depending on the complexity (e.g., single-root vs. multi-root teeth).
2. Gum Surgery (Periodontal Surgery)
In cases of advanced periodontal disease where deep pockets of infection exist between the gums and teeth, gum surgery may be required to remove the infected tissue and promote healing. This procedure may involve deep cleaning of the root surfaces, removal of infected tissue, or even bone grafts in severe cases of bone loss.
– Cost: Periodontal surgery can cost between $1,000 and $3,000 depending on the severity of the disease.
3. Root Canal Therapy
If a tooth is damaged but can be saved, root canal therapy is an option. This procedure removes infected pulp from inside the tooth, cleans the root canal, and seals it to prevent further infection. It is often used for fractured teeth or teeth with significant decay that haven’t affected the surrounding gums.
– Cost: Root canals can cost between $1,000 and $3,500, depending on the tooth involved and the severity of the infection.
4. Fractured Tooth Repair
If a dog has broken a tooth (for instance, by chewing on something hard), but the tooth can still be preserved, vets may recommend dental restoration. This could involve bonding or capping the tooth, similar to procedures in human dentistry.
– Cost: Tooth restoration ranges from $500 to $2,000 depending on the complexity.
5. Jaw Surgery
In rare cases of severe infection, trauma, or untreated dental disease, the dog’s jawbone may become affected, requiring surgery to repair or remove diseased sections of the bone. This is more invasive but may be necessary to save the dog’s life or prevent systemic infection.
– Cost: Jaw surgery can cost anywhere from $2,000 to $6,000, depending on the extent of damage and surgery complexity.
What Owners Need to Monitor Before and After Surgery
1. Before Surgery
– Appetite and Eating Habits: If your dog is showing reluctance to eat, especially hard kibble, or seems to be in pain when chewing, these are signs of advanced dental disease that may require surgical intervention.
– Oral Pain and Discomfort: Watch for signs of pain, such as pawing at the mouth, drooling, or a foul odor (halitosis) that won’t go away despite routine dental care.
– Swelling or Redness: Check for inflamed gums or swelling around the mouth, which could indicate a tooth abscess or gum infection.
– Behavioral Changes: If your dog becomes irritable or aggressive when touched around the mouth, this could be due to dental pain, signaling that the condition has worsened and may require surgery.
2. After Surgery
– Pain Management: Your vet will likely prescribe pain medications and antibiotics after surgery. Monitor your dog to ensure they are comfortable and not showing signs of excessive pain, such as whining, pacing, or reluctance to eat.
– Swelling and Bleeding: A little bleeding after tooth extraction or gum surgery is normal, but excessive bleeding or swelling could indicate complications. Keep an eye on your dog’s mouth and report any concerns to the vet immediately.
– Appetite: After dental surgery, dogs may have a reduced appetite due to soreness. Soft foods may be recommended during the recovery period. Monitor their eating habits closely to ensure they are still consuming enough calories to heal.
– Behavioral Changes: If your dog seems overly lethargic, refuses food for more than a day or two, or shows unusual aggression or depression, these could be signs of post-operative complications or pain. Contact the vet if you notice any of these symptoms.
3. Oral Hygiene Routine
After surgery, maintaining a proper oral care routine is critical to prevent future dental disease. Your vet will recommend regular tooth brushing, the use of dental chews, and possibly specialized oral rinses to keep your dog’s mouth healthy.
Information for Emergency Contacts
In the case of a dental emergency, such as a severe tooth fracture or abscess that could lead to a systemic infection, having a plan in place is vital. Here’s what information dog owners should have on hand for emergency veterinary care:
1. Medical History
– Dental History: Have a record of any past dental issues, treatments, or surgeries, including any extractions, root canals, or gum treatments.
– General Health: List any chronic conditions (like diabetes or heart disease) that may affect how the dog is treated or how well they tolerate anesthesia.
– Medication Record: Include current medications, especially if your dog is taking antibiotics, pain medications, or medications for other health conditions.
2. Emergency Vet Contact Information
– Primary Vet’s Contact: Include your vet’s phone number and address.
– Emergency Vet Clinics: Have the contact information for the nearest 24-hour emergency veterinary clinics in case your regular vet is unavailable after hours.
3. Important Symptoms to Report
– Pain: If your dog is whining, yelping, or showing signs of extreme discomfort, this is critical information.
– Swelling: Note any visible swelling in the face or gums, as this could indicate an abscess.
– Bleeding: Excessive or continuous bleeding in the mouth is a red flag, especially after trauma or recent dental work.
– Infection: Report any signs of infection, such as pus, foul odor, or a sudden change in your dog’s demeanor (lethargy, fever, etc.).
4. Recent Behavior
– Eating and Drinking: Inform the vet of any changes in your dog’s appetite, drinking habits, or reluctance to chew.
– Chewing Behavior: If the dental issue stems from chewing on something hard or inappropriate (bones, toys, etc.), mention this when you contact the vet. Knowing the cause can help them recommend appropriate treatments.
5. Insurance or Payment Information
If you have pet insurance, make sure you have the necessary policy information ready. Dental surgeries can be costly, so having insurance details can help expedite care.
Final Thoughts
Surgical intervention for dental disease in dogs can be lifesaving and dramatically improve their quality of life. Monitoring for signs of discomfort or disease, knowing when to seek professional help, and keeping detailed medical records are essential steps for owners. Having a dental care routine in place, and knowing what to expect before and after surgery, can make a significant difference in the overall health and well-being of the dog. By staying vigilant and prepared, owners can act quickly to address dental emergencies and ensure their pets receive the best care possible.